Dr. Haiquan Liu, Optometrist
What is Glaucoma?
Glaucoma is a group of diseases that damage optic nerve of the eye and result in blindness. According to WHO statistics, glaucoma is the second leading cause of blindness worldwide, and it is irreversible. It is estimated that 60 million people suffer from glaucomatous optic neuropathy and 8.4 million people are blind because of glaucoma. As cataract being the number one cause of blindness can be cured, glaucoma becomes the number one cause of irreversible vision loss. The chance of getting glaucoma increases with age. About one per cent of people between 45-50 years old, and about ten per cent of people over 80 develop glaucoma. Although the underlying mechanism of glaucoma is not fully understood, the main cause of glaucoma is associated with elevated pressure in the eye. Weakness in the optic nerve may also make it susceptible to the damage even the eye pressure within normal limits. In most cases, both factors are involved but to a varying extent.
What is Pressure in the Eye?
The eye is a relatively sealed ball shape organ. It requests certain pressure to maintain its relatively round shape and the pressure balance between eye ball and the blood pressure that supplies the eye. And please do not confuse the eye pressure with the blood pressure. The eye pressure is normalized by the balance of the production and the drainage of the clear fluid inside the eye which is called aqueous humour. The normal range of eye pressure is 10mmHg to 21mmHg. Aqueous humour is produced within a structure behind the iris, travels through the pupil. It brings nutrition to the transparent tissues, such as lens and cornea, then exits the eye ball through an angle formed by the cornea and the iris, and then through a structure called Trabecular Meshwork back to blood circulation. It is the imbalance of the production and the drainage of aqueous humour leads to elevated pressure inside the eye and causes glaucoma. How severe the glaucoma is will depend on how high pressure is, how long it has lasted, and whether there is a poor blood supply or other weakness of the optic nerve. A sudden elevated high pressure will damage the optic nerve immediately. A lower level of abnormal pressure can cause damage more slowly, and the vision would be lost gradually if the abnormal pressure is not treated in a timely manner.
What Are the Different Types of Glaucoma?
Based on the mechanism, glaucoma is usually divided into three main types of Glaucoma, namely primary glaucoma, secondary glaucoma and congenital glaucoma. In order to better understand the mechanism and the type of glaucoma, let’s assume there is a pump (ciliary body) continually pumps aqueous humour into the eye, and there is a half open door (angle formed by iris and the back of cornea) and a filter like structure (Trabecular meshwork) that drains and filters the aqueous humour out of the eye ball.
Primary Glaucoma
This is the most common type of glaucoma, with no other particular reasons found except the drainage system itself. There are two sub-types as indicated below.
Overall, this is the most common glaucoma. The door is open, but the filter is clotted. When the drainage channel becomes blocked slowly over years, the eye pressure rises slowly.
This type of glaucoma happens more often in the East Asia. The door is not open wide enough, and may close if there is a force pushes the iris forward. If the door is closed suddenly, it will cause pressure rise rapidly, that is called acute angle closure glaucoma. If the door is closed slowly overtime, it may cause chronic angle closure glaucoma. Chronic angle closure glaucoma is very similar to the primary open angle glaucoma.
Another rare type of angle closure glaucoma is Plateau iris syndrome, at which case the root of the iris is too short and alters the iris that blocks the angle (the door) at even younger age.
Secondary Glaucoma
The door or the filter is damaged or clotted by other eye conditions. It can develop from a complication of other medical conditions. They are sometimes associated with eye injuries, eye tumours, eye inflammation (Uvietis) or eye surgery. Advanced cataract can also cause secondary glaucoma. Using steroid, especially topically in the eye may induce glaucoma as well. Pseudoexfoliative glaucoma is the most common form of secondary open angle glaucoma associated with Pseudoexfoliation syndrome (PXF). It is a systemic condition characterized by the deposition of white protein-like material, called exfoliation material, within the anterior part of the eye and other organs. The deposition of this material in the trabecular meshwork can result in aqueous outflow obstruction. Pigmentary Glaucoma occurs when pigment from the iris flakes off and blocks the meshwork, blocks fluid drainage. Neovascular Glaucoma is a condition that neovascular and fibers grow in the angle and trabecular meshwork and blocks the draining system resulting in glaucoma. This condition is usually induced by diabetes and other ischemic retinal diseases, and it is hard to treat.
Congenital Glaucoma (Buphthalmos)
The door or the filter is not made correctly. The drainage system is not well developed or something goes wrong during the embryos development. It may happen in the eye only, or associated with other abnormalities. Majority of cases are diagnosed at infant stage. Some may happen in later life.
What Are the Risk Factors?
Although anyone can get glaucoma, some people are at a higher risk group than the others.
Primary Open Angle Glaucoma
Age: The older people have a higher chance to get glaucoma. As one per cent of people over the age of 40 -50 may be affected, and five per cent of people over the age of 65 may be affected.
Race: If you are of African origin, you are more at risk of chronic glaucoma and it may come on earlier and be more serious. Other origins, like African-American, Irish, Russian, Japanese, Hispanic, Inuit, or Scandinavian descent are also at high risk.
Family History: If you have a mother, father, brother or sister who has glaucoma, you are at high risk. You should have an eye test regularly, especially if you are over 40.
Short Sighted: People who are short sighted are more prone to glaucoma, especially when the short sight develops very fast.
Diabetes: Diabetes is believed to increase the risk of developing glaucoma.
Other risk factors like taking certain steroid medications, especially using steroid eye drop to control inflammation or allergy. Having had trauma to the eye or eyes may also cause secondary open angle glaucoma later on.
Primary Angle Closure Glaucoma
Age: Same risk as open angle glaucoma if you are over 40.
Race: East Asians are more susceptible to angle closure glaucoma. Inuit people are also at high risk.
Family history: If you have a first-degree relative who has angle closure glaucoma, then you have a higher chance to get angle closure glaucoma.
Far-sighted: Different from short sighted, far sighted people are at higher risk of developing angle closure glaucoma.
What Are the Symptoms of Glaucoma?
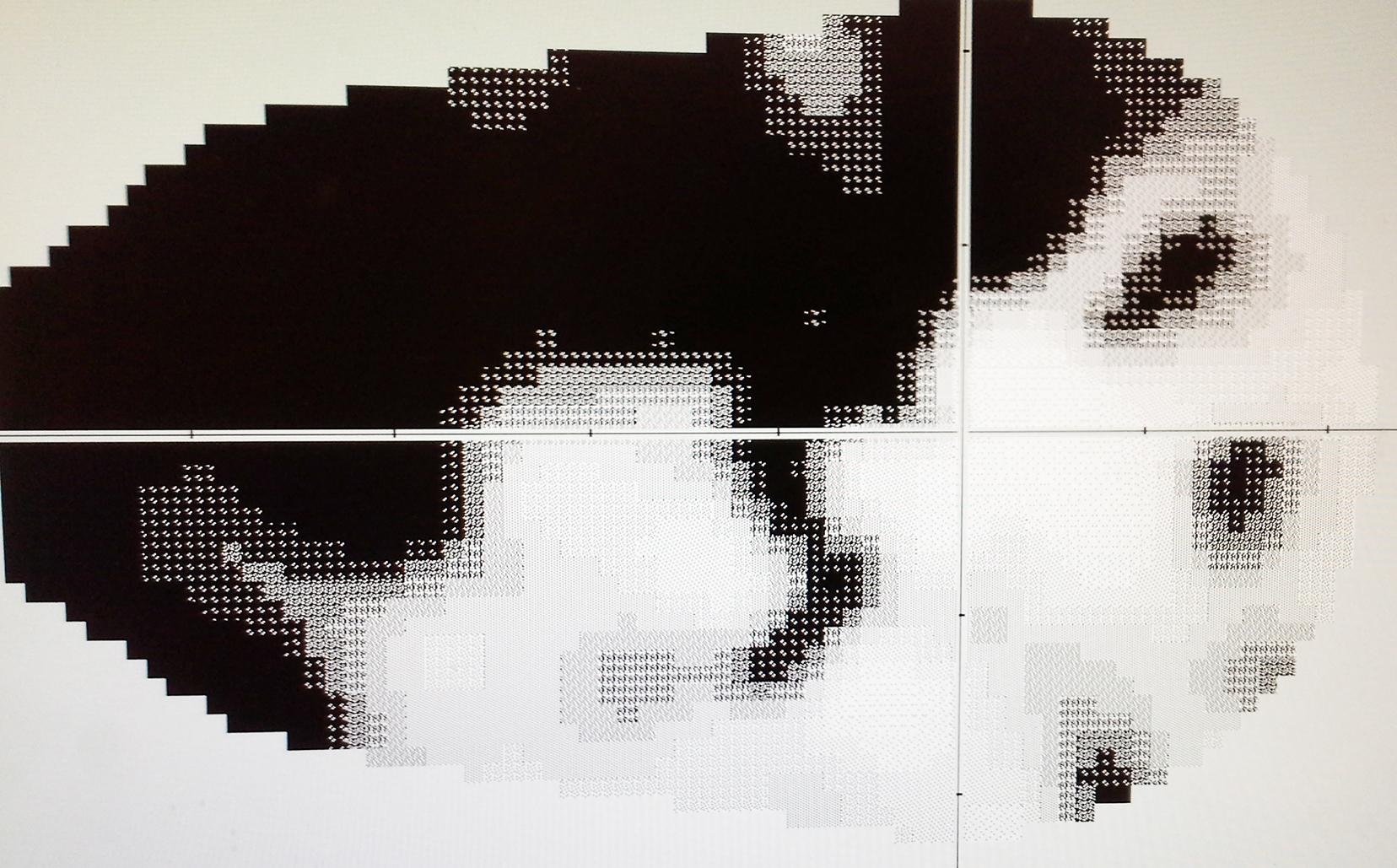
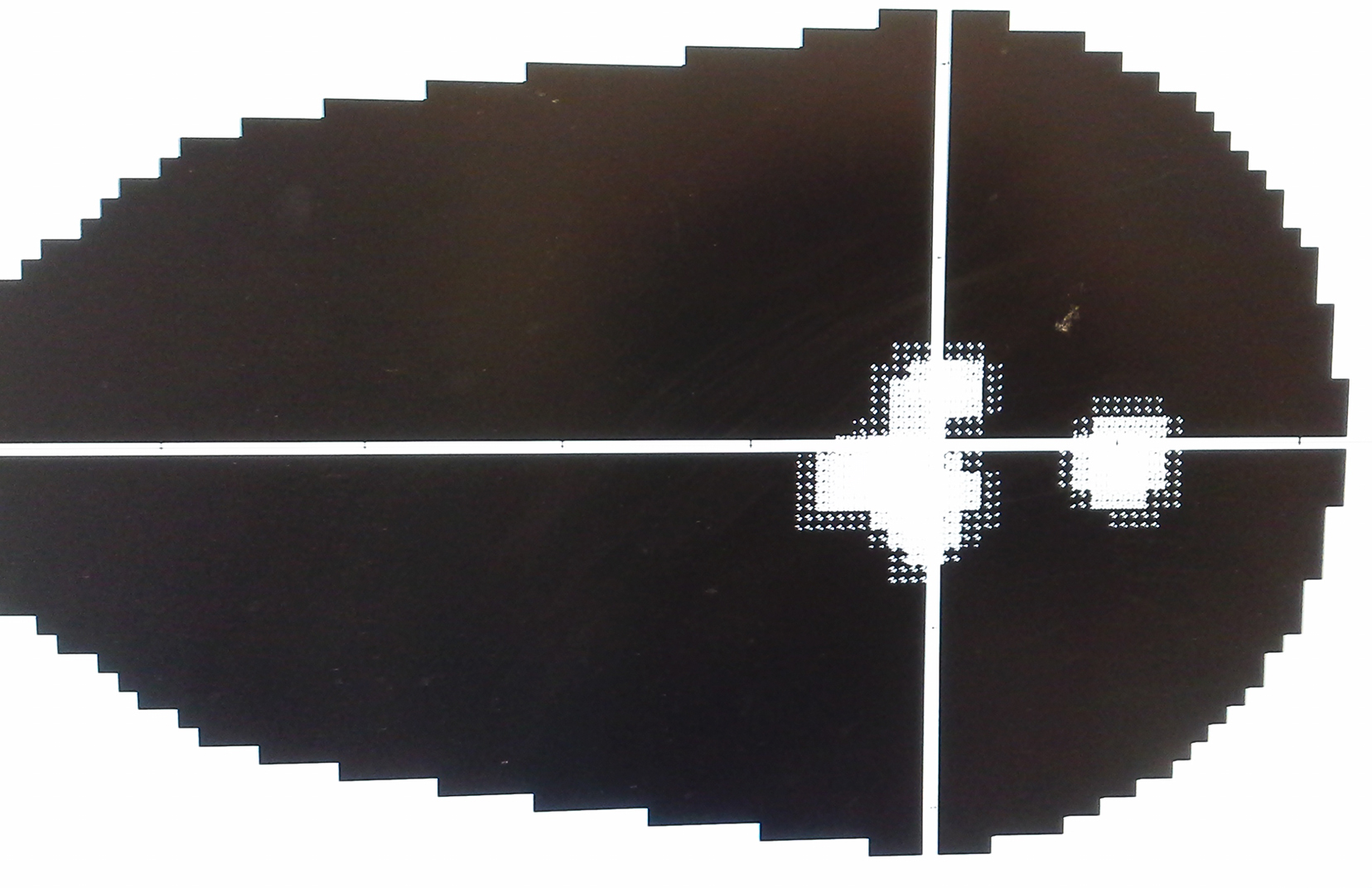
For the chronic glaucoma, as the eye pressure rises slowly and gradually, there are usually few or no symptoms. The first sign of glaucoma is often the loss of peripheral vision which can only be detected by computerized automatic visual field test. It can go unnoticed until late in the disease. This is why glaucoma is often called the "sneak thief of vision."
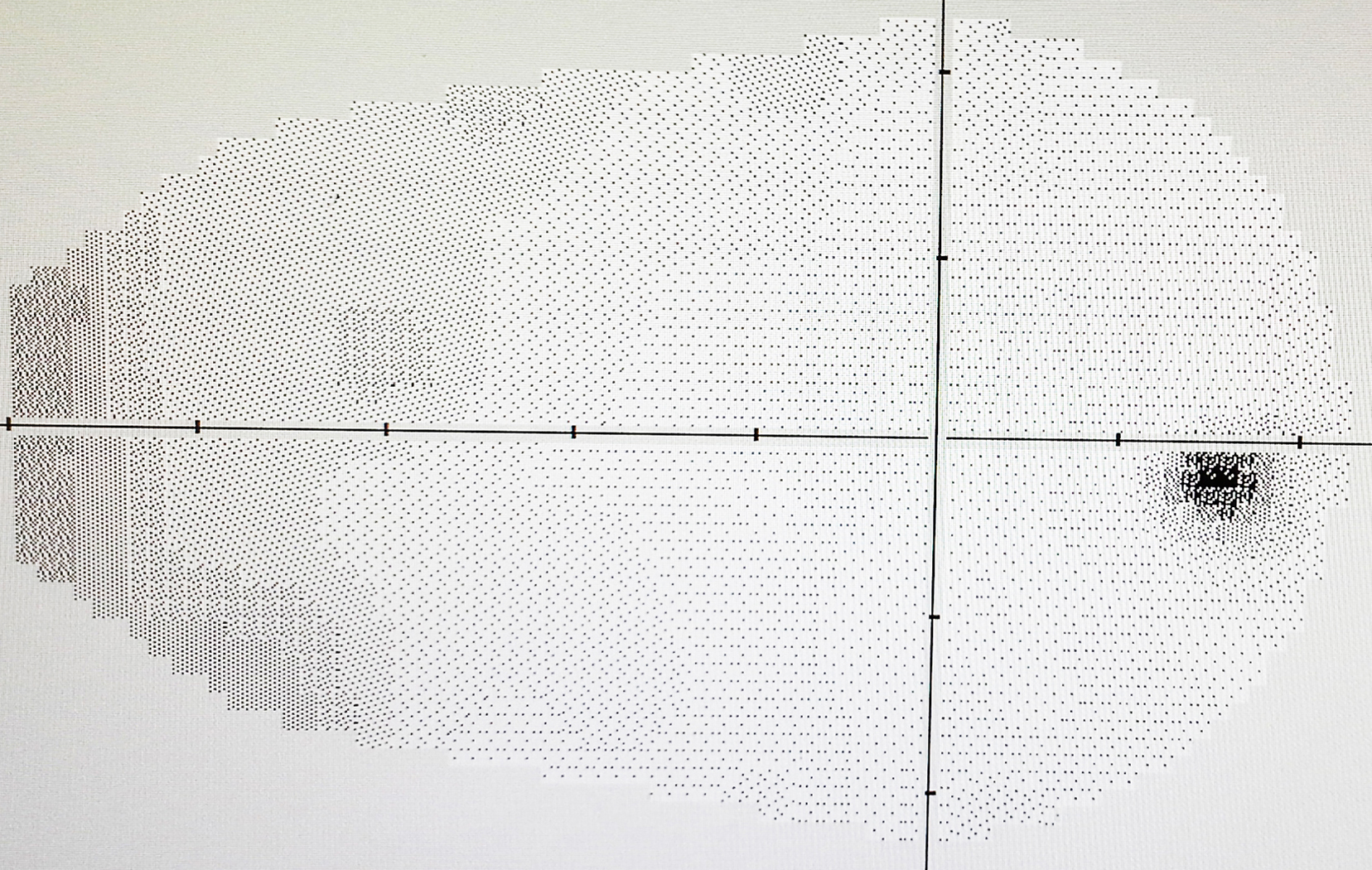
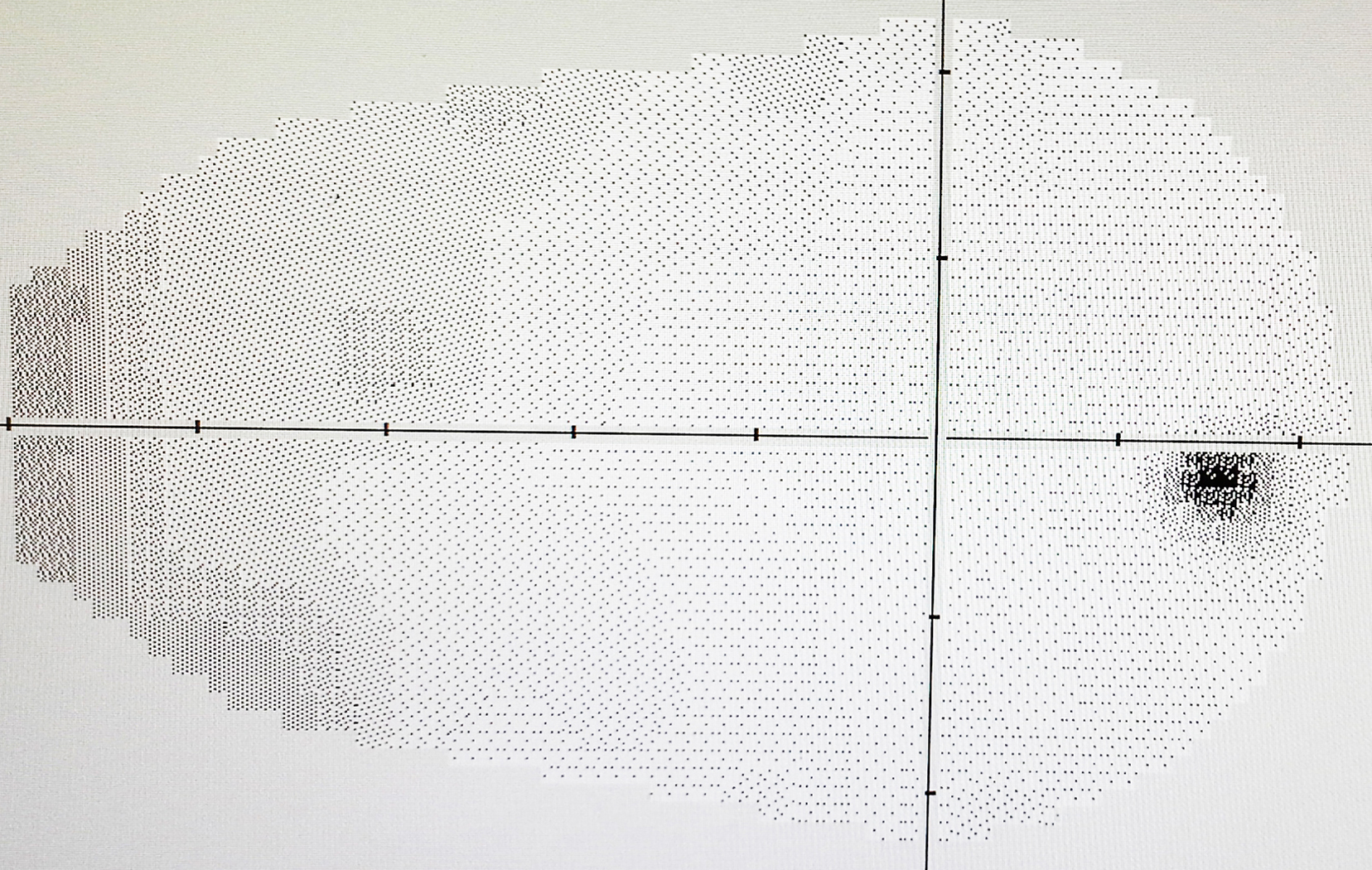
Normal visual field (VF)
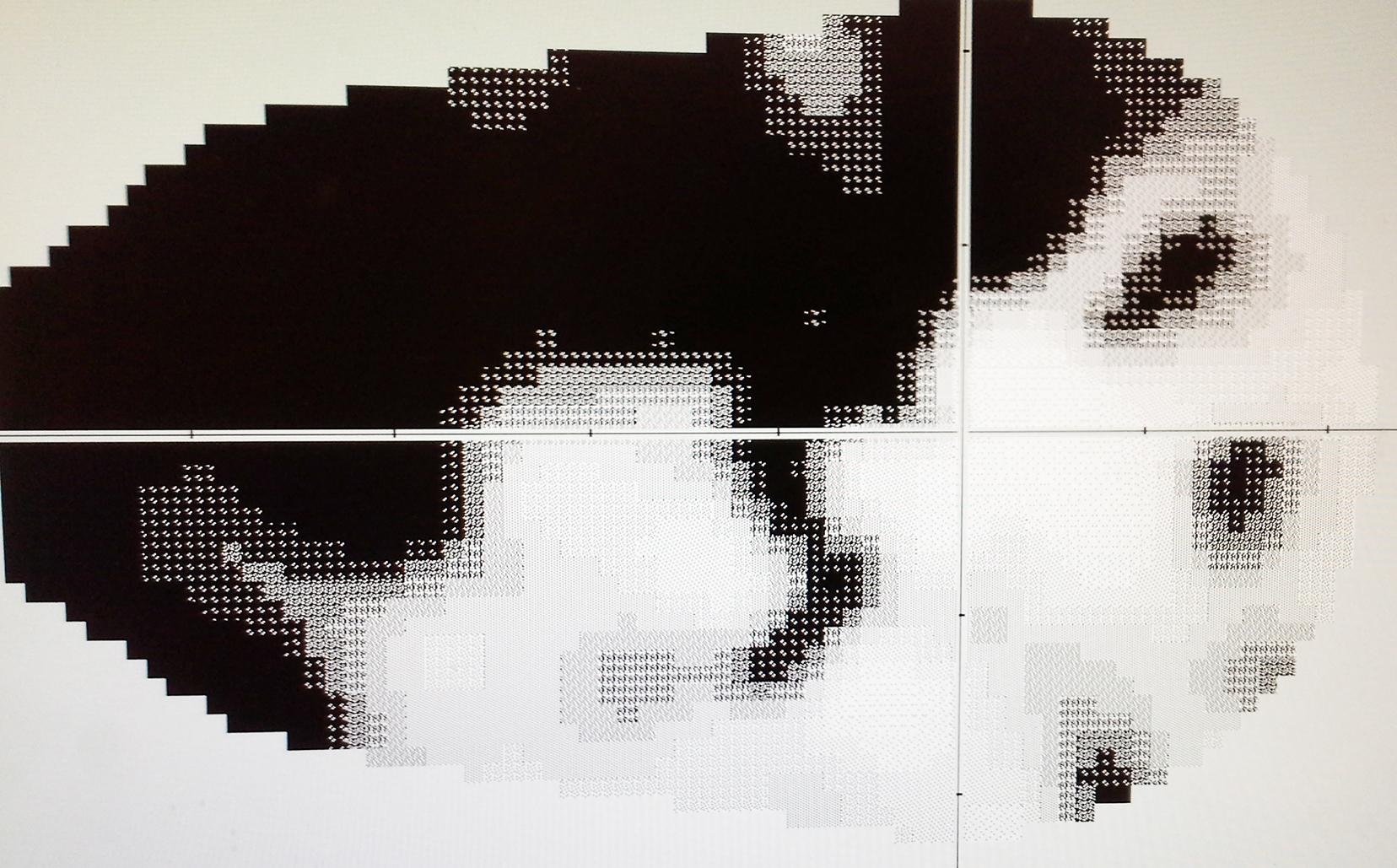
Advanced VF damage
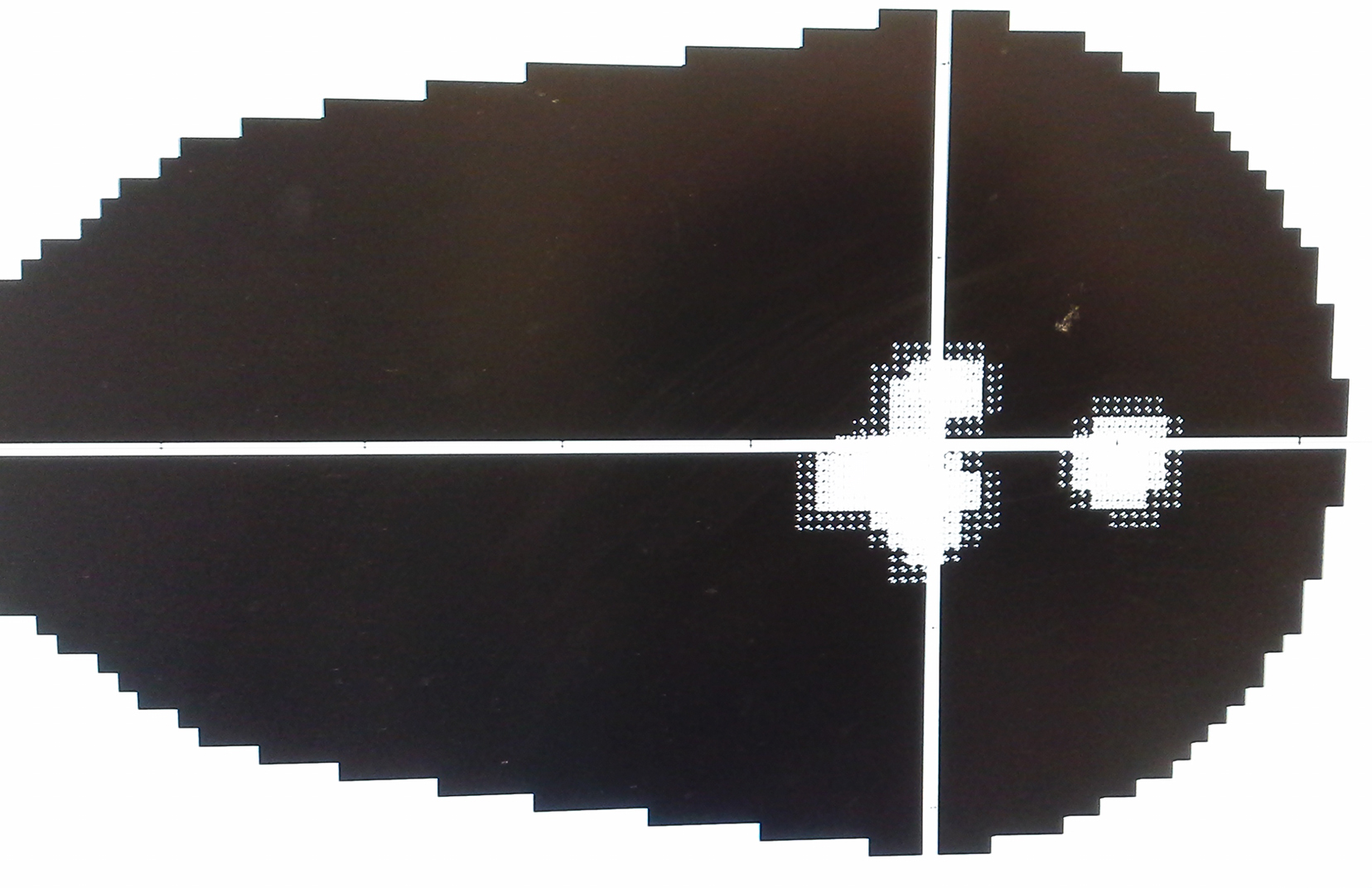
Endstage glaucoma VF
For the acute glaucoma, mainly in angle closure glaucoma, intraocular pressure can rise rapidly and dramatically, and can cause sudden eye pain, headache, blurred vision, or the appearance of halos around lights. It may also cause nausea and vomiting that can be mistaken as a cold or food poisoning. The eye becomes red, vision deteriorates and you may even faint. The acute glaucoma can be very painful and will cause permanent damage if it is not treated promptly. In some cases, angle closure glaucoma does not always cause sudden pain; you can have a series of mild attacks, often in the evening, and some discomfort in the eye, halos and hazy vision.
If you notice any of the following symptoms, you need to seek immediate medical care:
- Seeing halos around lights
- Vision loss
- Eye that looks hazy (particularly in infants)
- Nausea or vomiting with pain in the eye
- Narrowing of visual field (tunnel vision)
What Are The Usual Tests Involved?
As glaucoma becomes much more common over the age of 40, you should have a regular eye test with your eye doctor, optometrist or ophthalmologist, who will then carry out further tests as indicated below.
Pressure Test (Tonometry)
There are four types of pressure measurement
- Goldmann applanation tonometry:Gold standard, accurate, doctors or the technician need to receive special training to perform the test.
- Perkins Applanation Tonometry:A portable Goldmann applanation tonometer.
Goldmann Tonometry

- Schiotz Tonometer: Conventional and not use very often now.
- Tono-Pen: Easy and relative accurate
Rebound Tonometry: Non-contact, easy to perform, but relatively not accurate.
Pascal Dynamic Contour Tonometer: A new digital tonometry that provides a direct trans-corneal measurement of intra-ocular pressure (IOP), and is sensitive enough to detect the ocular pulse amplitude (OPA) due to the patient's heartbeat. It uses the principle of contour matching instead of applanation.
Optic Nerve Exam
The optic nerve can be viewed by a special instrument called direct or indirect ophthalmoscope. More accurately, laser optic nerve scan can measure the size and the volume of the optic nerve cupping and the nerve fiber layer thickness. The scan can provide the comparison of the optic nerve head and the nerve fibers. This information is very important when monitoring glaucoma patients.
Pachymetry
A small ultrasound prone is used to check the thickness of the central cornea as thinner cornea is susceptible to pressure damage.
Visual Field Test
A normal eye can see certain range of field when it focuses on one spot. Some diseases that affect the retina, optic nerve and visual pathway can cause visual field loss, glaucoma is one of them. There are some characteristics in early stage of glaucoma visual field damage which can only be detected by the computerized automatic parameter (visual field machine). It is a subjective exam, the patient needs to well understand the procedure and well cooperative to perform the test then the test result could be reliable. Other manual visual filed test ( Goldmann visual field test) is also available if the computerized automatic parameter is not reliable.
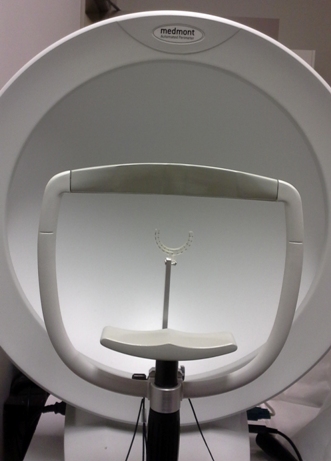
Visual field machine
Slit Lamp Microscope with Gonioscope
This exam will define it is angle closure or open angle glaucoma, as well as congenital glaucoma and sometimes the reasons of secondary glaucoma.
Gonioscope

What is Involved with Glaucoma Diagnosis?
Some patients are referred to glaucoma specialists, however, it does not mean she/he has glaucoma. Diagnosis of glaucoma is mainly based on the tests mentioned above. Normally, if the eye pressure is high, visual field defect corresponds with the optic nerve appearance and the nerve fiber loss, and then the glaucoma diagnosis is made. If some of the tests are abnormal while others are within normal range, the doctor may say you are a glaucoma suspect, and need to be followed regularly. Sometimes even the tests do not meet the diagnostic criteria, if the patient has several risk factors; the doctor may initiate the treatment as the nerve damage from glaucoma is irreversible. Sometimes, if the patient has narrow angle that makes her/him susceptible to angle closure glaucoma, a prophylactic laser peripheral iridoctomy is usually performed. Similarly, patient might not have glaucoma yet at this stage.
How Is Glaucoma Treated?
Since the main reason to cause glaucoma is elevated eye pressure, all the glaucoma treatments are mainly focus on lowering the pressure. If the pressure rises rapidly as it happens in acute glaucoma, the pressure needs to be lowered as soon as possible, or it will cause irreversible damage.
In the angle closure glaucoma, as there is a force to push the iris towards the cornea that closes the door, a hole will be by laser (called laser peripheral iridotomy) or by surgery ( called iridetomy, if laser is not available) at the peripheral of the iris to release the force. The remaining of the treatment is similar to the open angle glaucoma.
There are three methods to lower the pressure inside the eye, namely medication, laser and surgery.
Medications
Eye drops for glaucoma could either reduce the formation of aqueous humour in the eye or increase its outflow. There are five categories of eye drops. Prostaglandin analogs, including Xalatan, Lumigan and Travatan, are the kind of eye drops usually used as first line. If they do not work or patient develops allergy to them, then the doctor will consider the other eye drops.
Other eye drops are beta-receptor blocker, Alpha agonists, Carbonic anhydrase inhibitors (CAIs) and Cholinergic (Miotic). If one kind of eye drops works but the pressure is not lowered to the ideal level, the doctor may try another kind of eye drops. The eye drop combining the two different categories of glaucoma lowering agents into one is available as well.
Side effects of glaucoma eye drops may include allergy, redness of the eyes, headache, brief stinging, blurred vision, and irritation. Some glaucoma drugs may have systemic side effects that affect the cardio and respiratory system.
Other medications used systemically carry the similar side effects as the water pill and reduce the fluid in the body thus reduce the pressure in the eye.
Laser treatment
In angle closure glaucoma, laser is used to make a small hole in the iris (called laser peripheral iridotomy), allowing the fluid to flow from the posterior chamber to anterior chamber more freely, and releasing the force that pushes the iris towards the cornea.
In open angle glaucoma, laser is used to increase the outflow of the fluid from inside out (called trabeculoplasty).
The last laser treatment is used to partially destroy the structure that produces the fluid (called cyclophotocoagulation) if other methods do not work.
Surgery for Glaucoma
Surgery is mainly to create a new channel to drain the fluid out of the eye by either making a small hole on the eye ball or inserting a tube into the front part of eye ball, thereby reducing intraocular pressure that causes glaucoma. A conventional operation called trabeculectomy is the most commonly used one. Other techniques are employed to reduce the complication from the surgery. Sometimes this type of glaucoma surgery fails and must be redone. For some patients, a glaucoma valve (tube) implant is the best option. Complications of surgery for glaucoma include some temporary or permanent loss of vision, as well as bleeding or infection, cataract, etc.
Open-angle glaucoma is most commonly treated with various combinations of eye drops, laser trabeculoplasty, and surgery. Commonly, medications are used first, but some patients with glaucoma may respond better with early laser surgery or surgery.
Angle closure glaucoma is usually treated with laser iridotomy first, the rest of the treatment is similar to the open angle glaucoma.
Infant or congenital glaucoma is primarily treated with surgery, because the cause of the problem is the drainage system that is not developed properly.
Can Glaucoma Be Prevented?
Unfortunately, Open angle glaucoma cannot be prevented, but some of the angle closure glaucoma can be prevented if it is diagnosed and treated early.
At this time, loss of vision caused by glaucoma is irreversible and cannot be restored. However, successfully lowering eye pressure can help prevent further visual loss damage caused by glaucoma. Most people with glaucoma do not go blind if they follow their treatment plan and have regular eye exams.
Glaucoma can only be controlled but not cured, thus, glaucoma patients must follow up with their eye doctors regularly. Even the patients with narrow angle without glaucoma, when the prophylactic peripheral iridotomy is done, the risk of developing angle closure glaucoma is greatly reduced, yet, there is still a very small number of cases may develop angle closure glaucoma, therefore, the doctors may still want to follow up with the patient regularly.
Can Glaucoma Patient Drive?
Visual function for driving requirement varies from different Driver and Vehicle Licensing Authority in different countries. This will usually include certain visual acuity and visual field range, and some even includes color vision and binocular vision. The doctor will assess your visual function according to the regulations where you live and give you the answer. For a glaucoma patient, visual field will be the key concern if your best corrected visual acuity meets the driving requirement. If the loss of visual field is not advanced, most people can still drive.
What Happens if My Sight Cannot Be Fully Restored?
Early detection and prompt treatment usually prevents or slows further damage caused by glaucoma. There are many aids and equipments to help you utilize your remaining vision. You should ask your eye doctor about Low Vision Aids and whether you are eligible to register as partially sighted or blind. Registration enables you to get expert help and sometimes financial benefits such as tax reduction and getting a handicap parking permit.
The Canadian Health Awareness Society is a registered non-profit organization. Our Mission is to promote health awareness on health issues for all Canadians by education, support and advocacy.